
Journal of the Bahrain Medical Society
Year 2018, Volume 30, Issue 2, Pages 25-30
https://doi.org/10.26715/jbms.2_06082018Neale Nicola Kalis1*, Manal Al Taraif2
1Mohammed bin Khalifa bin Salman Al-Khalifa Cardiac Center (MKCC), Bahrain Defense Force Hospital, Kingdom of Bahrain.
2Royal College of Surgeons in Ireland, Dublin, Ireland.
*Corresponding author:
Neale Nicola Kalis, Mohammed bin Khalifa bin Salman Al-Khalifa Cardiac Center (MKCC) Bahrain Defense Force Hospital and RCSI (Bahrain), P. O. Box 28743, Kingdom of Bahrain; Tel: (+973)-17766959/(+973)-39048910, Fax: (+973)-17651112, Email: nnkalis@batelco.com.bh
Received date: April 08, 2018; Accepted date: August 06, 2018; Published date: September 21, 2018

Background and objectives: Fetal echocardiography is used for prenatal diagnosis of congenital cardiac malformations. The impact on the neonatal outcomes in the Middle East remains unknown; therefore, the study aimed to determine the impact of fetal echocardiography on short- and intermediateterm postnatal outcomes.
Methods: This is a retrospective case-control study, including 35 infants with a prenatal diagnosis of congenital heart defects (CHD). The cases were matched to 35 controls diagnosed postnatally with the same CHD. Demographic, clinical, and procedural variables were collected on a pretested form and compared. Statistical analysis was performed using SPSS 25.0. Contingency tables were created, and the grouped data were compared using the Fisher’s exact test.
Results: Mean age at diagnosis in the prenatal and postnatal diagnosed group was 1 day and 12.58 days, respectively (P = 0.001). In the prenatal group, 23 (65.71%) deliveries were performed in a tertiary healthcare setup compared to 13 (37.14%) in the postnatal group (P = 0.03). Duct-dependent CHD requiring prostaglandins was observed in 13 (41.94%) neonates in the prenatal group compared to 9 (28.13%) in the postnatal group (P = 0.3). There were 11 (31.43%) deaths in the prenatal group compared to 7 (20.00%) in the postnatal group (P = 0.4). There were no statistically significant differences among the procedural variables.
Conclusion: Fetal echocardiography aided in identifying neonates with complex CHD resulting in better parental counseling and delivery at a tertiary care center. However, this did not result in significantly short- and intermediate-term outcomes. Due to the small sample size, future follow-up studies are encouraged.
Keywords: Critical congenital heart defects; fetal echocardiography
Congenital birth defects (CBD) are the leading cause of infant mortality in developed countries.1 Congenital heart defects (CHD) constitute a major proportion of CBD. It is estimated that CHD contribute to almost one-half of the deaths, both as isolated lesions and as part of other multiple CBD.1
The prevalence of CHD remains static despite modern techniques and technologies to improve the ascertainment of cases.2
Prenatal fetal echocardiography (PFE) is now an accepted and accurate method of diagnosing CHD.3 It improves postnatal outcomes, especially in neonates who require prostaglandin infusion, such as patients with hypoplastic left heart syndrome (HPLHS)4 or transposition of the great arteries (TGA).5 The PFE is typically performed between 18 and 22 weeks of gestation.6 During the scan, a transducer is used to visualize the four-chambers of the heart, as well as the in-flow and out-flow tracts. PFE provides a comprehensive understanding of the structure of the fetal heart and allows identification of abnormalities, particularly, those missed during routine fetal screening.7
The Kingdom of Bahrain has a total population of over 1.2 million (census 2010)8 and the crude birth rate is 15.11/1000 people (2015).9 The latest recorded data validates 20,931 live births in the year 2014.10 According to data collected by the Mohammed bin Khalifa bin Salman Al-Khalifa Cardiac Center, the incidence of CHD is 14.9/1000 live births. To date, no study has been conducted to demonstrate the benefits of prenatal diagnosis of CHD in the Kingdom of Bahrain. Therefore, the study aimed to determine the impact of prenatal diagnoses using PFE on short- and intermediateterm outcomes in a tertiary pediatric cardiac center.
This is a retrospective case-control study, including 35 neonates (cases) born between 2003 and 2018, who underwent PFE and were diagnosed with CHD. The cases were matched with 35 controls with the same type of CHD who were diagnosed postnatally. Due to the retrospective design of the study, ethical approval was not necessary.
This is a retrospective case-control study, including 35 neonates (cases) born between 2003 and 2018, who underwent PFE and were diagnosed with CHD. The cases were matched with 35 controls with the same type of CHD who were diagnosed postnatally. Due to the retrospective design of the study, ethical approval was not necessary.
The data was analyzed using IBM SPSS 25.0; corrected mean values were calculated, where possible. Contingency tables were prepared, and the grouped data were compared using the Fisher’s exact test. The null hypothesis was rejected, if P < 0.05.
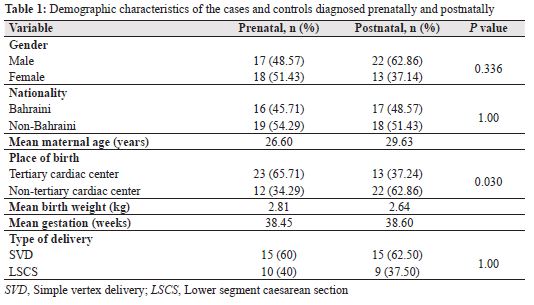
The variables, including sex, nationality, maternal age, birthweight, gestational age, and mode of delivery were not significantly different between the cases and controls (Table 1). However, a significant number of prenatally diagnosed neonates were born in a tertiary healthcare center when compared to those diagnosed postnatally (P = 0.030).
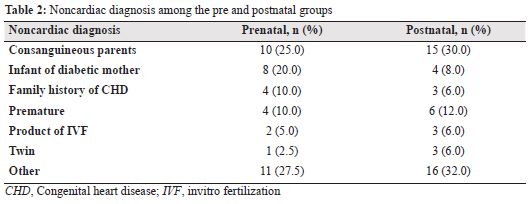
The main non-cardiac traits and/or diagnoses associated with both prenatal and postnatal groups included consanguineous parents, infant of a diabetic mother (IDM), prematurity, and family history of CHD (Table 2). Either of these traits were observed in 21 (60%) prenatally diagnosed and 22 (62.86%) postnatally diagnosed neonates (P = 1.0).
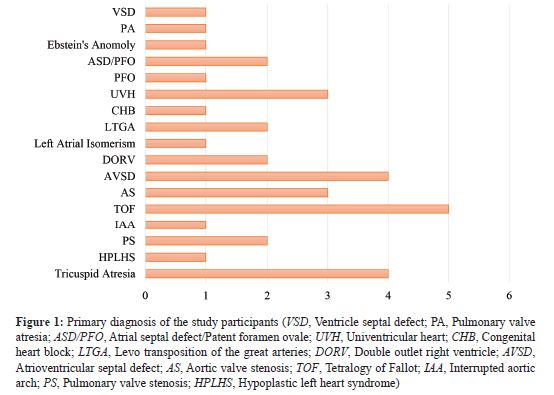
There were 17 different types of primary diagnoses ranging from minor non-critical CHD to critical complex CHD lesions (Figure 1). The mean age at confirmation of diagnosis using postnatal echocardiography in cases and controls was 1 day postnatal and 12.58 days, respectively (P = 0.001). In the prenatal group, patent ductus arteriosus (PDA)- dependent CHD was observed in 13 (41.94%) neonates and were treated with prostaglandins when compared to 9 (28.13%) neonates in the postnatal group (P = 0.3).
Although, there was a higher 11 (31.43%) overall mortality rate in the prenatal group when compared to the postnatal group 7 (20%), it was not significant (P = 0.4). In cases, 5 (14.29%) prenatally diagnosed neonates died during their first hospital admission as compared to 4 (11.43%) in the postnatally diagnosed group (P = 1.0).
The mean length of Neonatal Intensive Care Unit (NICU) stay in the cases and controls was 7.53 and 6.37 days, respectively. The mean length of total hospital stay was 11.21 and 7.78 days for the cases and controls, respectively.
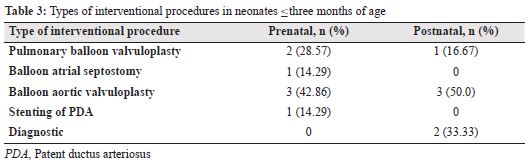
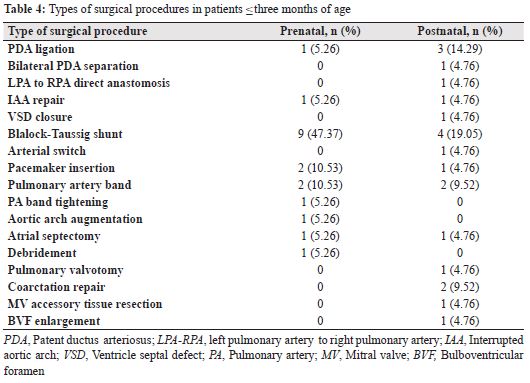
After their first admission, within the first three months of birth, one neonate each in the prenatally and postnatally diagnosed groups died (P = 1.0). One or more cardiac catheter interventional procedures within the first three months of life was observed in 4 (11.4%) and 5 (14.29%; P = 1.0) neonates in cases and controls, respectively. Among the cases and controls, 12 (36.36%) and 10 (28.57%) neonates, respectively, had one or more surgical procedures (P = 0.606) within the first three months of life (Tables 3 and 4). There was no significant difference in the number of readmissions between the two groups, with 1.25 and 1.23 readmissions in the prenatal and the postnatal groups. Equal number of neonates in the prenatal (15; 51.72%) and postnatal (15; 53.57%) groups are no longer on any medications (P = 1.0).
In the present study, a higher mortality rate was observed in neonates with a prenatal diagnosis when compared to those with a postnatal diagnosis. A similar study conducted in the Children’s Heart Centre, Mumbai explored the impact of fetal diagnosis on short and immediate-term outcomes. It was concluded that a prenatal diagnosis of CHD led to a decrease in morbidity and mortality as compared to a postnatal diagnosis. There was a higher mortality rate in the postnatal group compared to the prenatal group; most of the mortalities in the postnatal group occurred while transporting neonates to the tertiary healthcare center for treatment.11 This is in contrast to the findings of the present study, which can be explained with the geographical region of the Kingdom of Bahrain. Due to the small size of the country, easy and early transfer and transport can occur over short distances, which results in early and prompt diagnosis and a lower number of mortalities during the high-risk period of transit of those born without a prenatal diagnosis.
Most of the mortalities in our study occurred within the tertiary care center. Since interventional cardiology procedures can only be performed in the tertiary center, all infants who will require this treatment will, of necessity, be treated in the tertiary center. These procedures are inherently high risk, and this would explain the higher mortality.12
A large study conducted by Oster et al.13 examined the association of prenatal diagnosis of CHD with infant survival rates in the Metropolitan Atlanta Congenital Defects Program. Similar to our study, the study13 showed a significantly lower survival rate in prenatally diagnosed patients compared to those diagnosed postnatally. The higher mortality rate was mainly due to the number of isolated critical CHD lesions, which were more likely to be prenatally diagnosed than the isolated non-critical CHD lesions. Additionally, their results showed that there was no significant difference in survival rates between the prenatally and postnatally diagnosed patients with isolated non-critical CHD lesions. This correlates with our study, as the more complex nature of the critical CHD might explain the higher mortality rate in our prenatally diagnosed patients and makes it more likely that the parents will choose tertiary healthcare centers. However, performing a study to test this assumption would be difficult, as our tertiary healthcare center database does not provide data regarding the severity of the CHD lesion in each patient.
We had hypothesized that a prenatal diagnosis of CHD would lead to an improvement in the postnatal short- and intermediate-term outcomes. However, unexpectedly, our results showed a slightly higher mortality rate, longer hospital stay, and higher rate of prostaglandins use in the prenatally diagnosed group when compared to those diagnosed postnatally. This indicates slightly worse outcomes and proves our primary hypothesis false.
A statistically significant number of the mothers in the prenatal group chose to give birth in the tertiary healthcare center (P = 0.0306). This allowed for better preparation and counselling of the parents, which has shown to improve the psychological impact on the mother, leaving her less likely to blame herself or the neonate’s father for the fetal abnormality.14 It also allowed for better planning and preparation of the time and mode of delivery, as well as NICU awareness.
The present study showed that prenatal diagnosis of CHD allows the multi-disciplinary team to be better prepared for the birth-related complications and to counsel the parents beforehand. This could lead to more admissions to the tertiary healthcare center resulting in improved treatment during pre and postnatal periods. However, this does not reflect a statistically significant improvement in the mortality rates or overall short and intermediateterm outcomes in the Kingdom of Bahrain.
There were several limitations in the study. Due to the retrospective study design, the cardiac database used did not contain all information required for the patients in both the prenatal and postnatal groups. Additionally, it was not possible to calculate P values for the mean values, as the SPSS statistics program required a minimum of 2 × 2 contingency table.
In case of suspicion of any cardiac abnormality during routine gestational ultrasound, the patient should be referred for a detailed fetal echocardiography scan at a tertiary healthcare center to rule out CHD.
Patients diagnosed with complex CHD in the fetal echocardiography scan should have a planned delivery in a tertiary healthcare center. This would ensure the highest level of safety and optimize the stability of the neonate during the perinatal period.
The authors of the study have no conflict of interest to declare.