
Journal of the Bahrain Medical Society
Year 2018, Volume 30, Issue 3, Pages 42-51
https://doi.org/10.26715/jbms.3_30102018Heba Al Saad*, Ashish Mhatter
King Hamad University Hospital, P.O.BOX: 24343, Busaiteen, Kingdom of Bahrain.
*Corresponding author:
Heba Al Saad, King Hamad University Hospital, P.O.BOX: 24343, Busaiteen, Kingdom of Bahrain., Tel.: (+973) 33369677, Email: Heba.al.saad.94@gmail.com
Received date: July 14, 2018; Accepted date: October 30, 2018; Published date: December 31, 2018

Various prospective randomized controlled trials were conducted to compare open and laparoscopic appendectomies. The aim of this systematic review is to compare both the surgical appendectomy interventions and to evaluate the most favored, safe, and effective choice of treatment for appendicitis. In this review, 2462 studies have been retrieved from three major databases: Medline, Scopus, and Cochrane. The inclusion criteria were clinical diagnosis of appendicitis, publication date, and patient’s age. Of these, six studies that met both inclusion and exclusion criteria were chosen. The studies selected were assessed for quality using the CONSORT PRO tool. The data extracted was later analyzed using NCCS 2007 software and Microsoft excel. The means and P values were calculated using the student t test and chi square test provided by the studies. The six studies chosen met the inclusion criteria and achieved an average quality of 15.5 over 25, which is in line with the CONSORT PRO tool. The results indicated that further elaboration on the randomization method should’ve been provided; however, the methodology was the same across the six studies showing a strong correlation and homogeneity in the outcomes. The primary outcomes were all favored in laparoscopic appendectomy (LA) except for intra-abdominal abscesses. The secondary outcomes were all favored by LA exceptfor cost and mortality, which weren’t favored by both the interventions. In conclusion, LA is a safer and more effective surgical procedure than open appendectomy.
Keywords: Appendectomy, laparoscopy, open surgery, outcomes, prospective studies, randomized controlled trials
The point of tenderness in a ruptured appendix was first determined by Charles McBurney in 1889.1 Appendectomy using McBurney’s incision was established due to his work and remained the treatment of choice for appendicitis until 1983. Kurst Semm provided another method of surgery, known as laparoscopic appendectomy (LA). Thirty-three years later both surgical procedures are under application.1, 2
There have been several controversies over the different types of treatments. Some suggest that open appendectomies (OA) are better due to its success in comorbid patients; while, others suggest that LAs are better due to the fewer complications and less pain and duration of hospital stay.3, 4
In Bahrain, the number of appendectomies is increasing, and LA is, almost, always the treatment of choice. In this systematic review, the two methods of surgery are compared, which has rarely been done before. Therefore, it would be good oppurtunity to determine which intervention is the most favored, safe, and effective choice of treatment.
The studies were selected based on the following criteria: patients aged ≥ 12 years with appendicitis, the diagnosis was made clinically with a history of pain in right iliac fossa or periumbilical region shifting to the right iliac fossa, nausea/vomiting, physical examination (tenderness and guarding), increased white cells count (more than 10000/dL), and positive radiological imaging. Moreover, the studies included the outcomes needed for the review (duration of stay in hours, postoperative pain, wound infection, and postoperative complications).5-10 Full-text, prospective randomized controlled trials (RCTs) that performed LAs with the three-port technique and published in the last 10 years in English language were included in this review.
Studies with the following exclusion criteria were exempted from this review to prevent bias: previous history of lower abdominal surgery, patients denying informed written consent, and pregnant patients.
Primary outcomes were duration of stay in hours, postoperative pain, wound infection, and intra-abdominal abscesses. Secondary outcomes were complications, time until return to work in days, mortality, quality of life (QoL), and cost.
Studies published between January 2006 and January 2016 were identified from various databases and journals, such as Medline (generated through EBSCO and PubMed), Scopus, Cochrane database, and Google scholar. Certain studies were selected from journals, such as “The Saudi Journal of Gastroenterology” and “Journal of Clinical and Diagnostic Research”. All the studies were approved by the Ethical Committee in the respective hospital.
Search results were screened by one author independently based on title, abstract, and full text to identify relevant RCTs according to the inclusion criteria. The studies selected were prospective RCT’s; other studies such as, cohort studies and retrospective studies were excluded to prevent major heterogeneity between the RCTs. If the RCTs were duplicated, the one with the most complete inclusion and exclusion criteria was included. The same author assessed the quality of the studies using the CONSORT PRO tool. A supervisor overviewed the quality and screening of the RCTs included in the review. Any disagreement was resolved by consensus. If there were still some unresolved discrepancies, a third reviewer was involved in the discussion.
The following data were extracted from each study: general data (the author, year of publication, and journal), study characteristics (study design and setting), and patients’ characteristics (age and number of subjects per group). Only two studies included the patients’ body mass index (kg/m2) and American Society of Anesthesiology score I/II/III. Primary and secondary outcomes were extracted from each study and provided in tables. Pain was assessed through the visual analogue score by the authors, which was also extracted for this systematic review. The extracted data was qualitatively analyzed through tables and flow charts.
The quality assessment of the six studies was done using the CONSORT PRO tool. Consort Pro provides a checklist allowing a proper assessment of the study topics (abstract, introduction, methods, results, and discussion) along with its outcomes. Each assessment question was rated “yes”, “no”, or ‘’not applicable (NA)”.
Most of the studies followed the checklist in terms of the abstract, introduction, and methods. Some points weren’t applicable to this study, such as changing the method after the trial had commenced. Additionally, most of the studies didn’t elaborate on the randomization method, for instance some didn’t mention the blinding process, while others didn’t mention the randomization method. Certain points in the CONSORT PRO tool, such as binary outcomes and reason behind ending a trial weren’t applicable.
All analyses were performed using Microsoft Excel. Outcomes were sorted out as primary and secondary to reduce heterogeneity. A table, including demographic baseline was created to provide an overview of the patients’ characteristics and the appropriateness of the sample chosen by the authors regarding this systematic review.
The sample size for the selected studies was based on the main parameters (duration of stay in hours, return to work in days, pain, wound infection, and intra-abdominal abscesses).
The P value of each RCT was extracted; authors used chi-square test, students t test, and Mann-Whitney test to calculate it. Authors considered P value < 0.05 as statistically significant, and they also provided the confidence interval for the results retrieved. The student t test was used to analyze the set of data between LA and OA and were statistically significant from each other in all the studies. The methodology of each RCT was analyzed to test for heterogeneity. The mean difference in outcomes was calculated for continuous variable (duration of hospital stay in hours).
Various search terminologies were used to broaden the results, such as ‘open appendectomy’, ‘laparoscopic appendectomy’, ‘duration of stay’, ‘primary outcomes’, ‘postoperative pain’, ‘complication’, ‘wound infection’, ‘hospitalization stay’, ‘intra-abdominal abscess’, ‘mortality’, ‘time of return to work’, and ‘quality of life’. The keywords were used in Medline, Scopus databases, and journals. Boolean operators allowed the combination of different terminologies together such as, ‘‘open’’ OR ‘‘laparoscopic’’ AND ‘‘appendectomy” to broaden the search. The database was then filtered according to age (young adults and above), type of publication (RCT and prospective), species (humans), language (English), publication dates (last 10 years), and free text.
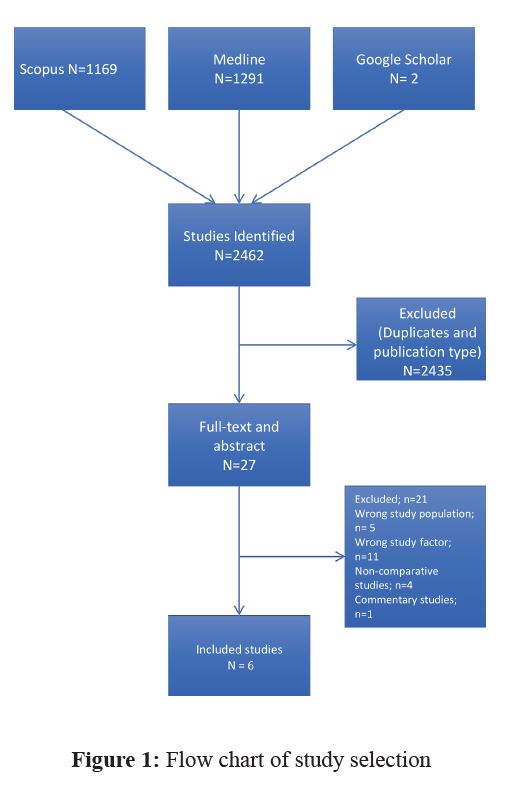
The initial literature search identified 1169, 1291, and 2 studies from Medline, Scopus database, and Google scholar, respectively, giving a total of 2462 studies. A total of 2435 studies were excluded due to their publication type (retrospective RCTs) and duplication (being repeated in different databases), while 27 were selected for title, abstract, or full-text review. After exclusion of 21 studies due to inappropriate population (children aged 6–11 years), wrong study factors (not focusing on the outcomes needed for this review but focusing on factors such as, the best antibiotic for effective recovery), commentary (not providing sufficient evidence), and being noncomparative, therefore, only six studies were included for the systematic review (Figure 1).

![]()
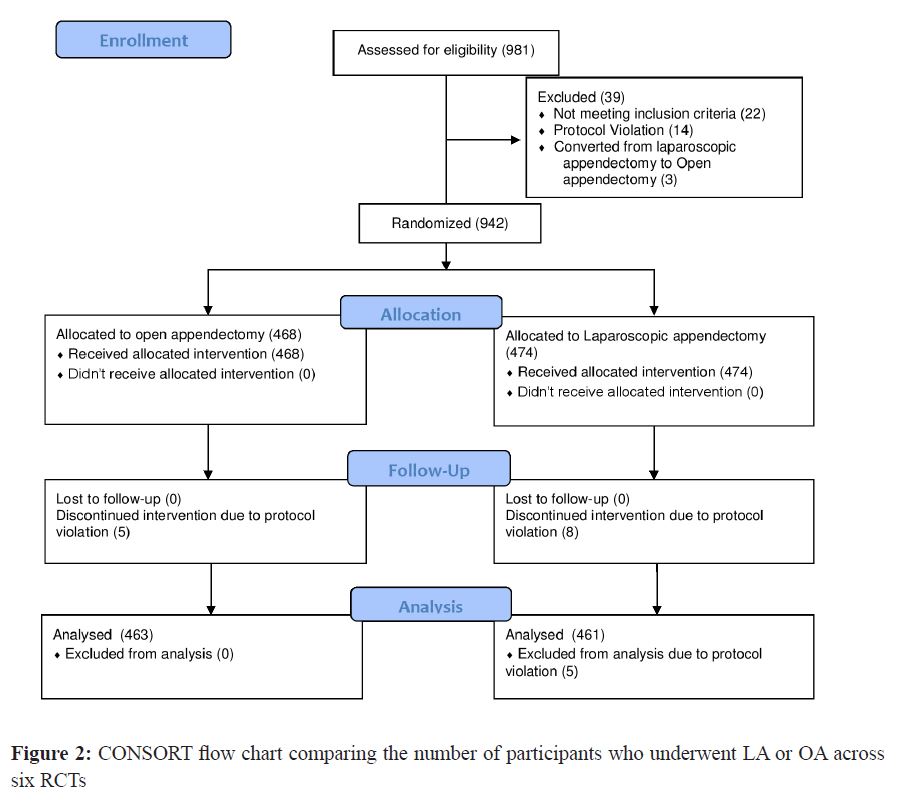
The six studies selected for this systematic review consisted a total of 981 patients; 39 patients were excluded due to protocol violation, not meeting the inclusion criteria, and conversion from LA to OA. Of the remaining 942 patients, 468 underwent OA and 474 underwent LA. Five and eight patients who underwent OA and LA, respectively were excluded due to protocol violation. The total count reduced to 463 and 466 patients in OA and LA groups, respectively. Finally, five patients scheduled for LA didn’t meet the protocol, and 461 patients were analyzed. However, the reason for protocol violation wasn’t mentioned to avoid bias in all six studies (Figure 2).
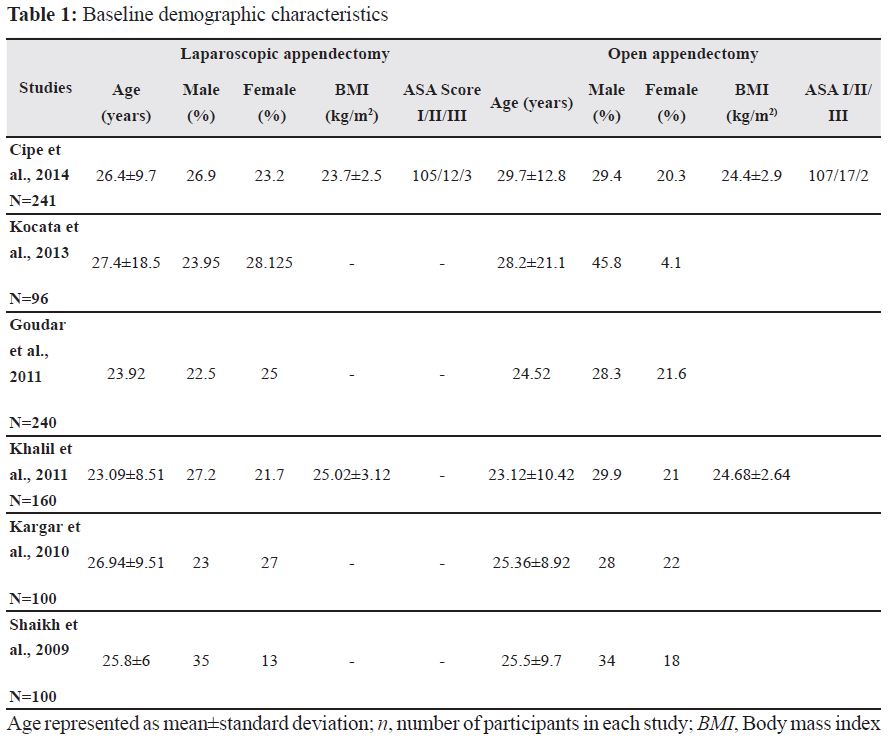
All six studies were comparative, prospective RCTs; two each from Turkey and Pakistan and one each from India and Iran. The mean age of the patients who underwent LA and OA was 25.5 years and 26.07 years, respectively. Patients were diagnosed with appendicitis before undergoing any procedure. Two studies included the patients’ body mass index (kg/m2) and American Society of Anesthesiology score I/II/III (Table 1).
All the studies provided the information needed to assess its quality (Table 2). The assessment of ‘outcome’ was marked as ‘P’ in the CONSORT PRO checklist where Kocata et al. (2013), Goudar et al. (2011), and Khalil et al. (2011) mentioned them as primary and secondary outcomes, whereas Cipe et al. (2014), Kargar et al. (2010), and Shaikh et al. (2009) did not mention.

All surgical procedures across the six studies were performed based on the same protocol. Surgeons used the three-trocar technique to perform LA, whereas, OAs were performed with same standard technique. The patients were treated with anesthesia for the pain, and discharged when they were on a regular diet and afebrile. All patients across the six studies were followed up for 1 month and informed to report any postoperative complication.
While some studies used diclofenac sodium (75 mg) as an analgesic, others used per-oral naproxen sodium (550 mg twice a day) and one study used morphine. The use of different medications for postoperative pain causes heterogeneity in visual analogue score, which represents the severity of postoperative pain. This produces heterogeneity in the outcomes results. However, all the studies used the same prophylactic dose of third generation cephalosporin and metronidazole, attaining a strong correlation and homogeneity in the results of wound infections.
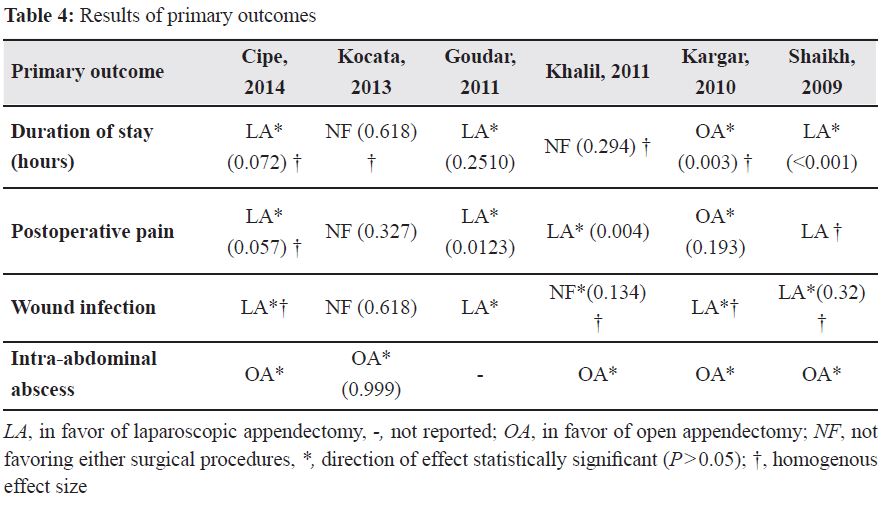
In the primary outcomes, three studies favored LA in terms of duration of stay, one favored OA, and two other studies disapproved either of the treatments. In four studies, postoperative pain was better managed with LA, while one study favored OA and another study didn’t favor either interventions (Table 3).

Wound infection was less in patients undergoing LA, while two studies didn’t approve either interventions (Kocata et al. study wasn’t statistically significant). However, intra-abdominal abscesses were less in patients who underwent OA; OA was favored by five studies (Table 4).
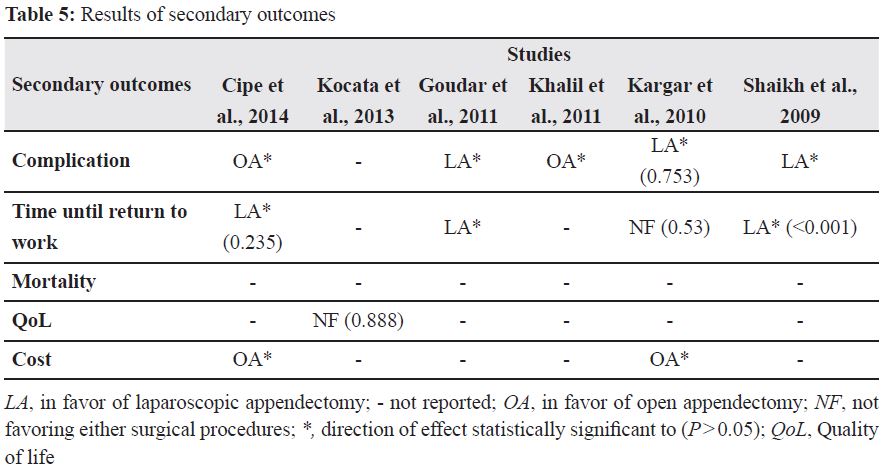
In terms of the secondary outcomes, complications were less in patients who underwent LA; two studies favored OA, while one study didn’t report the complications. Time of return to work was better in LA, it was favored by three studies; whereas, one study didn’t favor either interventions. Mortality was not observed in either procedure, quality of life was better in patients who underwent LA, and cost was less in OA (Table 5).
Discussion
The results of this systematic review show that the duration of stay in the hospital was less in LA by 16.365 hours, which permits early return to work and the efficient QoL of patients. Further, it enables a better healthcare service with faster emergency operations for patients and reduced risk of mortality. Wound infections were almost three times higher in patients who underwent OA. This indicates a better infection control and prevention of the risk of opportunistic infections in immune-compromised patients who undergo LA.
However, the incidence of abscess is higher in LA patients than in OA. According to the six studies, most of the patients who underwent LA were previously suspected of having a complicated appendicitis. This definitely increases the chances of OA being favored in this specific outcome. Furthermore, intra-abdominal abscess may also occur due to the type of surgery and in diabetic and immune-compromised patients.11 Nevertheless, this cannot be entirely concluded from the studies due to the inclusion criteria, which was that patients had to be of normal body mass index (kg/m2) range and should be free of any comorbidities. Additionally, precautions must be considered for patients with high risk of infection, such as diabetics, immune-compromised, and elderly patients, when LA is considered as the treatment of choice.
Time until return to work was favored in LA procedure; Cipe et al. and Shaikh et al. reported that LA patients return to work 1–2 days earlier than OA patients. In addition, Goudar et al. suggested that OA takes 7 days more than LA before any patient is able to go back to work. As opposed to OA, this is a great advantage to LA as it prevents patients from being delayed for work, and so, it won’t greatly affect the patients financially. The OA procedure exemplifies the cost of duration of stay and the hospital as there will be additional follow ups, more analgesics, and increased time needed to get appointments of doctors.
Postoperative complications, such as vomiting, paralytic ileus, wound dehiscence, intra-abdominal abscess, small bowel obstruction, and bleeding were almost twice as high in OA than LA, across all six studies. This is the main reason why patients undergoing OA need a longer duration of hospital stay and the time needed to return to work is prolonged, causing OA to be more costly, ineffective, as well as risky.
Reduced postoperative pain has been favored by all the studies for LA procedure except for KARGAR, which has preferred OA and reported less postoperative pain. The study’s authors explained that this could have been an effect of not blinding the patients, the whole pain scale was subjective to the patient and that all LA patients have experienced pain located in the shoulder as opposed to OA. The shoulder pain is specific to LA due to the phrenic nerve irritation to the diaphragm caused by the carbon dioxide gas remaining postoperatively.12 The results of Karagar et al. were statistically insignificant (P = 0.193).
According to Karagar et al. and Cipe et al., the disadvantage in LA procedure is the higher cost due to the use of new technologies while operating. However, it might not be possible for a patient with a low socioeconomic class to undergo the procedure. It’s a fact that the cost of OA is cheaper in the short term when compared to LA. Most systematic reviews have shown that the cost of OA is relatively equivalent to LA in the long term as the increased cost of hospital stay in OA procedure balances the expenses equation. Due to this reason some studies have shown that there isn’t a significant difference in the cost between the two surgical interventions.13-15
Therefore, all the factors show positive results for LA procedure: shorter duration of hospital stay; less postoperative pain, wound infection, and complications; better QoL; and early return to work. Mortality was not observed in either of the surgical procedures. OA procedure is only favorable for its costs and fewer intra-abdominal abscesses. However, this is due to the fact that the patients were suspected of a complicated appendicitis in all the LAs done across all the six studies, which increases the chances of abscess formation in LA as opposed to the noncomplicated appendicitis in OA. This can further be proven through various studies indicating ‘appendectomy recovery’ suggesting that LA has a shorter hospital stay (leaving the hospital within 24 hours), smaller incision leading to fewer wound infections, less postoperative pain, and minimal complications (hernia). The study further elucidates that even though the risk outweighs the benefits in OA, many patients prefer OA due to increased cost in LA.
According to the literature, OA has many known complications, such as infection, which include wound infections, abdominal abscess, peritonitis, adhesions, and fecal fistula. Furthermore, it has some disadvantages, such as increase in the duration of hospital stay, postoperative pain, and time return to work.16, 17
In 2017 a research concluded that LA is better than OA with respect to the wound infection, duration of hospital stay, earlier return to normal activity, better cosmetic appeal, and lesser use of antibiotics.18 Most studies chose LA to be the golden standard for any appendectomy due to its safe and more effective surgical approach than OA. Except for Kocata et al. who have stated that ‘laparoscopic approach to appendectomy for patient with uncomplicated appendicitis doesn’t offer a significant advantage over the open approach’. This has been concluded due to the fact that the studies had lower number of participants (96: 46 in OA and 50 in LA), which won’t show a major statistical difference in the results.
The main limitation that occurred in this systematic review is the change of procedure from LA to OA, which was included in the results of three studies. Ultimately changing the randomization number, which could have affected the outcomes of each study negatively. All primary and secondary outcomes weren’t reported by the six studies and that causes a limitation; one study didn’t mention intra-abdominal abscesses, while another didn’t mention the complication and five didn’t mention the QoL results. The third limitation is the use of different medications by various RCTs, such as the use of different analgesia and antibiotics that could cause a high risk of bias and heterogeneity in between the studies. The fourth limitation is that the studies didn’t mention other factors, such as duration of the surgery, which is an important parameter displaying a good comparison between the two surgical interventions.
The strengths of this systematic review were: reporting the severity of appendicitis by all six studies, therefore, the benefits of each intervention were accurately measured. All the studies were prospective RCTs preventing heterogeneity. The methodology chosen by all six studies was similar resulting in a stronger correlation between outcomes and homogeneity. Other factors, such as children under the age of 12 and comorbid patients that could have been the limitations, were omitted, given that all the six studies had the same exclusion criteria. Another strength would be the similar protocols followed by six studies; they all used the same techniques to perform both OAs and LAs. All the patients were fully informed and taken consent before any procedure was taken. A thorough follow-up was accomplished, and patients were sedated during both the surgical interventions.
The weaknesses of this systematic review are: all of the studies chosen are published only in English and the studies that were published in other languages were omitted; the nature of all the six studies was prospective; and other studies, such as retrospective and cohort studies were not included to avoid heterogeneity and bias.
A meta-analysis wasn’t done in this systematic review since the topic was a qualitative topic. According to the CONSORT PRO tool, details on the randomization method, such as blinding features and control groups should have been mentioned by all six studies. However, according to the SHAM surgical intervention, certain steps that are considered important in therapeutic RCTs can be omitted in surgical RCTs, for instance it would be considered unethical to blind the patient and surgeon due to the fact that the subjects are humans. Therefore, this step isn’t done in the six RCTs. The control group here is the OA group, it’s considered as a ‘fake’ or ‘sham surgical’ control group in surgical RCTs as it wouldn’t be ethical to blind surgeons and patients from surgical interventions.19, 20
Various systematic reviews conducted to evaluate the same topic, focused particularly on the duration of hospital stay. Most of them reached to the same conclusion that LA is the gold standard treatment (intervention) for appendicitis. The limitation in those reviews was the SHAM surgical intervention implemented in surgical RCTs.21-27
The surgical guidelines (SAGES) recommend that any surgeon about to perform an intervention on appendicitis, the first choice should always be LA instead of OA to prevent the spread of infection, which goes hand in hand with the CDC guidelines.28, 29
Due to the guidelines, systematic reviews, RCTs, and other studies, LA is increasingly becoming the main intervention chosen for the treatment of the disease despite its cost and intra-abdominal abscess formation.
Conclusion
In this systematic review a comparison was done between LA and OA procedures through numerous prospective RCTs. When compared to OA, LA is more advantageous, safe, and has significant benefits with improved QoL. Thus, this review concludes that LA is more effective and safer than OA; LA should be the gold standard surgical procedure for most patients diagnosed with appendicitis.
This study would like to recommend that more RCTs and systematic reviews should be conducted regarding the difference between the single-port LA and three-port LA to evaluate which intervention provides the best treatment for appendicitis, which is a topic that hasn’t been addressed by many studies.
Conflicts of interest
The authors of the study have no conflicts of interest to declare.